Need help covering medical transport costs? Here’s what you need to know:
- Medicaid: Offers broad Non-Emergency Medical Transportation (NEMT) benefits. Eligibility depends on income, state rules, and medical necessity.
- Medicare: Original Medicare only covers ambulance rides for emergencies or certified medical need. Some Medicare Advantage plans include NEMT benefits.
- Private Insurance: Rarely covers routine medical transport unless it’s medically necessary and pre-approved. Coverage varies by provider.
Key steps to save on transport costs:
- Confirm coverage with your insurer.
- Follow pre-authorization rules.
- Use in-network transportation providers.
Transportation shouldn’t stop you from getting care. Check your policy today and secure affordable, reliable rides to your appointments.
Non-Emergency Medical Transportation Insurance | Do you need it?
Medicaid Coverage for Medical Transportation

Medicaid stands out as a key program providing Non-Emergency Medical Transportation (NEMT) benefits, ensuring individuals can access essential healthcare services. Since Medicaid is managed at the state level, the specific rules and procedures for these benefits can vary depending on where you live. Below, we’ll break down eligibility requirements and the types of services covered to help you navigate these benefits.
Who Qualifies for Medicaid NEMT Benefits
To take advantage of NEMT benefits, you must first be enrolled in Medicaid. This program offers health coverage to several groups, including children, pregnant women, parents, and seniors. For most participants, financial eligibility is determined using the Modified Adjusted Gross Income (MAGI) method. However, for those applying based on blindness, disability, or being 65 or older, income is assessed through the Supplemental Security Income (SSI) program guidelines.
Some individuals automatically qualify for Medicaid, such as those enrolled in SSI, participants in the breast and cervical cancer treatment program, children with adoption assistance agreements under Title IV-E, and young adults who meet the criteria as former foster care recipients. Additionally, beneficiaries must be residents of the state where they’re applying and must be either U.S. citizens or qualified non-citizens. Many states also offer programs for medically needy individuals, allowing people with significant healthcare needs to "spend down" their income on medical expenses until they meet Medicaid’s financial requirements.
Once enrolled, you can access NEMT benefits if you meet two key conditions: you don’t have another way to get to your medical appointments, and the transportation is for medically necessary services covered under your Medicaid plan. Let’s take a closer look at what these services include.
Services Covered Under Medicaid
Medicaid NEMT benefits cover transportation for appointments deemed medically necessary under your state’s Medicaid guidelines. The specifics of what’s covered – such as the types of transportation and the nature of the trips – depend on the rules laid out by your state’s Medicaid plan and your individual coverage.
How to Use Medicaid NEMT Benefits
Once you’ve confirmed your Medicaid eligibility, here’s how to access NEMT services. Start by checking with your state Medicaid agency to understand the process. Since each state operates its program differently, follow the instructions on your Medicaid card or visit your state’s official Medicaid website for details. If you encounter any issues, contact your state Medicaid office directly for assistance.
Medicare Coverage for Medical Transportation
Medicare has stricter rules for routine transportation compared to Medicaid. Knowing what Original Medicare covers – and what it doesn’t – can help you avoid surprise bills and explore other options, such as Medicare Advantage plans. Below, we’ll break down what’s covered under Original Medicare and the expanded benefits often available through Medicare Advantage.
Original Medicare Coverage Limits
Original Medicare (Parts A and B) does not cover routine, non-emergency transportation. So, if you need a ride to a regular doctor’s appointment or checkup, you’ll likely need to pay out of pocket or look into other coverage options.
However, Medicare Part B does cover ambulance transport when it’s deemed medically necessary. For instance, if you’re undergoing treatments like dialysis or chemotherapy, Medicare may pay for ambulance services – but only if a doctor provides written documentation certifying it as medically necessary. Without this certification, Medicare won’t reimburse the cost.
It’s important to understand that this coverage is limited to ambulance services. Medicare does not pay for other types of vehicles, like standard cars or wheelchair vans, even if they’re needed for essential medical care.
Medicare Advantage Plans and NEMT Benefits
Medicare Advantage plans (Part C) often fill the gaps left by Original Medicare. Many of these plans include non-emergency medical transportation (NEMT) benefits, which are not covered under Original Medicare. These benefits can vary widely depending on the plan, your location, and the provider. Not every Medicare Advantage plan offers NEMT coverage, so it’s crucial to review your plan details or contact your insurer to confirm what’s included.
If your plan does provide NEMT benefits, you’ll need to follow a few steps to use them. First, talk to your doctor to obtain a certification of medical necessity. Once you have the required documentation, reach out to your Medicare Advantage plan coordinator or a Medicare-approved transportation provider to arrange your rides.
For more information about transportation benefits, visit the official Medicare website or call 1-800-MEDICARE (1-800-633-4227) for assistance.
sbb-itb-8e5d2ef
Private Insurance Coverage Options
When it comes to private health insurance, non-emergency medical transportation (NEMT) is rarely included as a standard benefit. Unlike Medicaid, which typically covers NEMT, most private insurers view routine transportation as something patients need to handle on their own. However, there are exceptions – some insurers may cover transportation if it’s for specialized medical services that aren’t available locally and deemed medically necessary. The specifics often hinge on the insurer’s policies.
The best way to determine whether your private insurance covers NEMT is to contact your insurance provider directly. Ask about your policy’s coverage limits, eligibility requirements, and whether pre-authorization is needed. This step can help you understand how private insurance fits into your overall plan for managing transportation-related expenses.
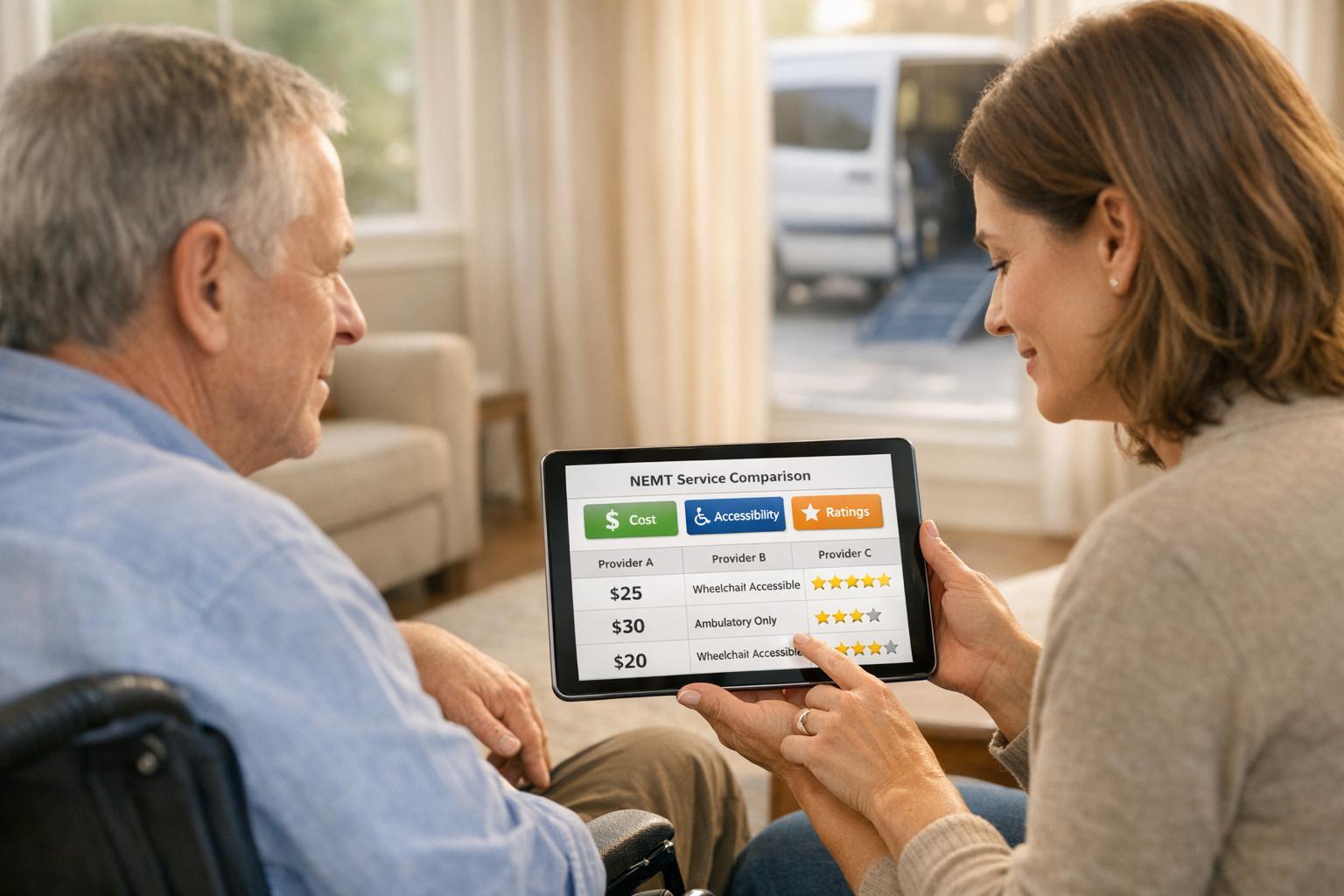
How to Reduce Out-of-Pocket NEMT Costs
Planning ahead can make a big difference when it comes to cutting down transportation expenses. By understanding your insurance benefits and following the necessary steps before scheduling a ride, you can keep your out-of-pocket costs to a minimum.
Verify Coverage and Get Pre-Authorization
Before booking a ride, take the time to confirm your insurance coverage. This simple step can save you from unexpected bills. Reach out to your insurance provider to learn about your Non-Emergency Medical Transportation (NEMT) benefits, including any limitations and the requirements for a medically necessary trip.
Make sure you have important details on hand, such as your Medicaid ID, Social Security number, medical records, and identification. If you’re on a Medicaid health plan, call the transportation number provided by your plan. If not, use your state’s general NEMT program line – for instance, in Texas, you can call 877-633-8747.
It’s also essential to request pre-authorization well in advance. For appointments within your county, aim to do this at least two business days before your visit. For out-of-county trips, plan ahead by at least five days. If your appointment is on a Monday, make sure to call no later than the previous Thursday.
When scheduling the ride, have all the necessary information ready, including your full name, address, phone number, member ID, appointment type, date and time, pickup address, and your provider’s contact details. If you need special accommodations, such as a wheelchair-accessible vehicle, make sure to mention it. Some programs may also require you to confirm that no other transportation options are available. Following these steps can help avoid claim denials. This is particularly important for those with private insurance, as NEMT benefits vary widely and often come with strict criteria.
Once your coverage is verified, check that the provider is in-network to help keep your costs down.
Use In-Network Providers
Choosing in-network providers is another effective way to lower expenses. For Medicaid recipients, using approved NEMT providers ensures your ride is covered, which can significantly reduce or even eliminate out-of-pocket costs.
To find approved providers, contact your county’s transportation broker. For example, in Washington State, the Health Care Authority offers a directory of transportation brokers by county. Your Medicaid caseworker can also provide guidance on coverage details and available transportation options.
If you have private insurance, it’s especially important to confirm that your chosen provider meets your insurer’s requirements. Carefully review your policy to understand any transportation benefits, including the criteria providers must meet. Don’t hesitate to reach out to your insurance company directly for help finding covered providers and understanding what documentation you’ll need.
Conclusion
Understanding your insurance options can make a big difference when it comes to managing medical transport costs. Medicaid provides broad non-emergency medical transportation (NEMT) benefits, while Original Medicare limits coverage to medically necessary ambulance services. Medicare Advantage plans often bridge that gap by including additional transportation benefits. Private insurance and supplemental policies differ greatly, so it’s important to carefully review your plan to know what’s covered.
To make the most of these options, take a few proactive steps. Contact your insurance provider to confirm your benefits, follow any pre-authorization requirements, and stick to in-network providers to keep costs in check. Keep a detailed record of your medical appointments and transportation needs, and if a claim is denied, gather the necessary documentation to file an appeal.
Your insurance can be the key to affordable and reliable medical transport. Missing appointments not only affects your health but can also lead to higher costs down the road. By taking advantage of the benefits available in your plan, you can ensure safe and cost-effective transportation to your medical appointments.
Reach out to your insurer today, verify your NEMT coverage, and take the necessary steps to secure dependable transport.
FAQs
Does my Medicare Advantage plan cover Non-Emergency Medical Transportation (NEMT)?
To determine whether your Medicare Advantage plan offers Non-Emergency Medical Transportation (NEMT) benefits, begin by checking the benefits summary that comes with your plan. This document usually lists covered services, including transportation for medical appointments.
If the details are unclear or you have questions, reach out to your plan’s customer service team. They can confirm if NEMT is included, explain any eligibility rules, and walk you through how to use the service. Don’t forget to ask about possible costs, like copayments or limits on the number of trips covered.
What can I do if my private insurance doesn’t cover non-emergency medical transportation?
If your private insurance doesn’t cover non-emergency medical transportation (NEMT), don’t worry – there are alternative options to explore. Medicaid and Medicare may cover NEMT services, but it depends on your eligibility and the specifics of your plan. To find out what’s available, contact your state’s Medicaid office or your Medicare provider for detailed information and guidance on how to apply.
Another option is to look into supplemental insurance policies that include transportation benefits. These plans can help ease the financial burden of getting to routine medical appointments or treatments. Additionally, some local programs or community organizations may provide low-cost or even free transportation services for those who meet their criteria.
Take the time to carefully review your current insurance policy and reach out to your provider to confirm what’s included. They can also guide you on any additional resources or options that might be available to help with transportation costs.
Who qualifies for Medicaid’s Non-Emergency Medical Transportation (NEMT) services?
Medicaid offers Non-Emergency Medical Transportation (NEMT) services to individuals who are unable to use regular transportation because of medical or physical limitations. These services are designed to ensure beneficiaries can safely and reliably reach their medical appointments. However, a healthcare provider must determine that the service is necessary.
Since eligibility rules and covered services can differ by state, it’s essential to review the details of your specific Medicaid plan to understand what’s included and how to arrange transportation.