Getting patients with mobility challenges to medical appointments in Austin requires careful planning, compliance with laws, and specialized services. Non-Emergency Medical Transportation (NEMT) providers help bridge gaps in access, ensuring safe, timely, and dignified travel for those with disabilities or medical needs. Key practices include:
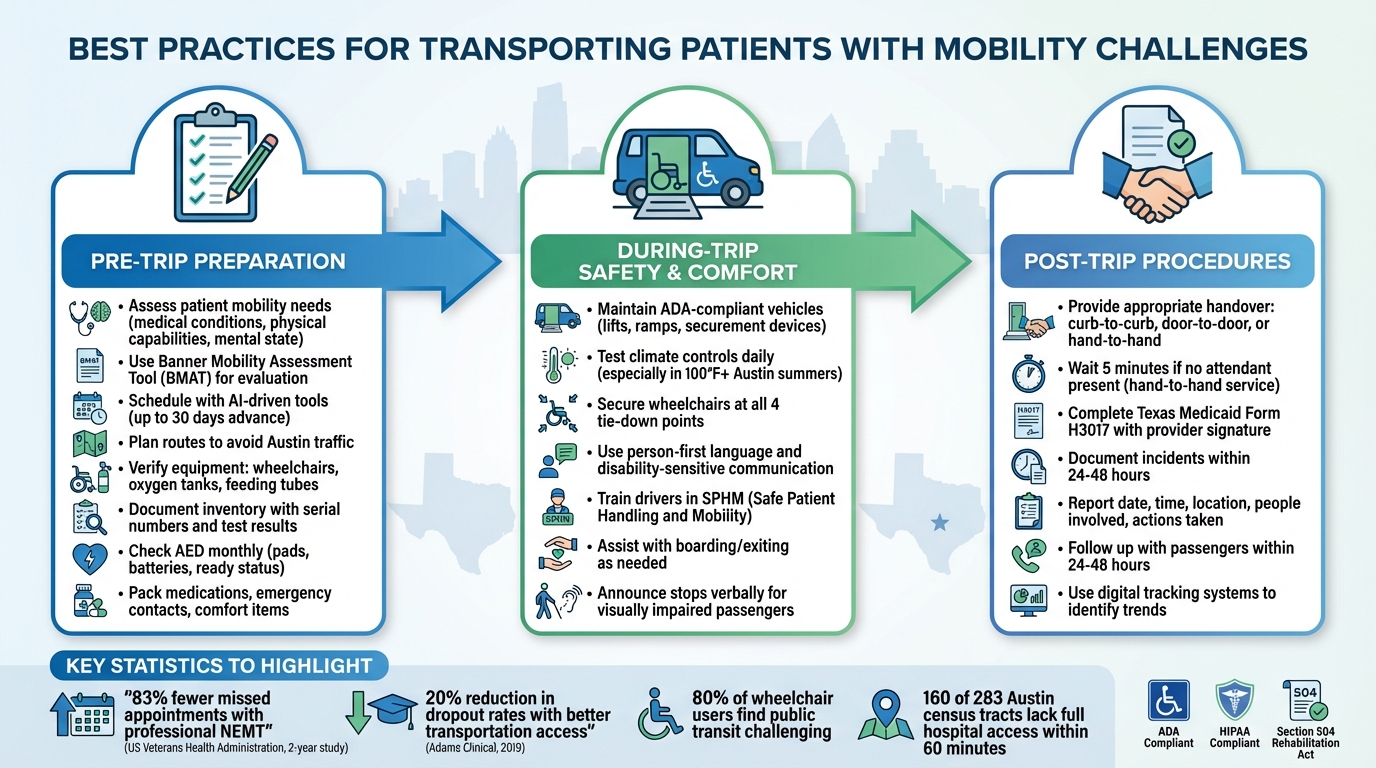
- Pre-Trip Preparation: Assess patient needs, plan routes to avoid Austin’s traffic, and ensure equipment like wheelchairs or oxygen tanks is ready.
- During-Trip Safety: Maintain ADA-compliant vehicles, secure patients properly, and train drivers for effective communication and care.
- Post-Trip Follow-Up: Ensure safe handoffs at destinations, document trips, and address incidents promptly to improve service.
Austin’s traffic and uneven healthcare facility distribution pose challenges, but tools like AI scheduling and trained staff help mitigate these issues. Providers must also comply with ADA and HIPAA standards to protect patient rights and data. Services like Zyvra Mobility exemplify how professional NEMT can improve healthcare access and reduce missed appointments.
Best Practices for Safe Patient Transportation: Pre-Trip, During-Trip, and Post-Trip Procedures
How To Transfer patients between a Wheelchair & Vehicle – by SingHealth Community Hospitals
Common Challenges in Transporting Patients with Mobility Issues in Austin
Transporting patients with mobility challenges in Austin comes with its fair share of hurdles. From navigating the city’s layout and traffic to meeting strict regulatory standards, ensuring safe and dignified transportation requires careful planning and execution.
Austin’s Traffic and Healthcare Facility Layout
Austin’s notorious traffic congestion is a major obstacle, especially during weekday mornings when medical appointments are often scheduled. Delays caused by heavy traffic can make it difficult for patients to arrive on time for critical procedures or treatments.
Adding to the complexity is the distribution of healthcare facilities across the city. Most hospitals are concentrated in central and north-central Austin, leaving peripheral areas – particularly in the eastern and western parts – underserved. A December 2024 study by Yang and Wang highlights this issue: out of 283 census tracts in Austin, only 123 have full public transit access to hospitals within a 60-minute travel time. The remaining 160 tracts are either partially covered or completely without access, with 72 of the partially covered tracts having less than 50% coverage.
This lack of access disproportionately impacts vulnerable communities. For example, in eastern Austin, 13 of the 35 uncovered tracts have Hispanic or Latino populations exceeding 50%.
"When we talk with our patients, we hear that inadequate transportation is often a barrier to accessing health care." – Sarah Cook, CCC Director of Integrated Delivery System Strategy and Planning
These challenges underscore the urgent need to expand accessible transportation options in underserved areas. However, geographic and logistical concerns are only part of the equation – regulatory requirements also play a significant role.
ADA and HIPAA Compliance Requirements
Beyond traffic and location issues, transportation providers must navigate stringent regulatory standards. The Americans with Disabilities Act (ADA) mandates that medical services, including transportation, be fully accessible to individuals with disabilities. Similarly, Section 504 of the Rehabilitation Act of 1973 extends these protections to federally funded programs.
To comply with these standards, providers must ensure their vehicles are ADA-compliant, facilitate safe boarding for patients, and properly train their staff. As CapMetro states:
"No qualified individual with a disability shall be excluded from participation in, denied the benefits of, or subjected to discrimination under any program, service, or activity provided by a public entity, solely on the basis of their disability."
On top of ADA requirements, providers must also adhere to HIPAA regulations, which protect patient data throughout the transportation process. This involves using secure systems and procedures to safeguard sensitive information. Healthcare providers coordinating non-emergency medical transportation must ensure their services meet both ADA accessibility standards and HIPAA privacy requirements[1]. Failure to comply can result in legal penalties, loss of federal funding, and damage to the provider’s reputation – making these standards essential for any legitimate transportation service.
Pre-Trip Preparation Best Practices
Getting everything in order before a trip is essential to avoid delays and ensure patient safety, especially when navigating Austin’s well-known transportation challenges. Taking the time to assess patient needs, plan routes thoughtfully, and confirm equipment readiness can make all the difference in providing a smooth, safe, and comfortable experience.
Assessing Patient Mobility Needs
Understanding a patient’s mobility requirements goes beyond a simple "yes" or "no" about wheelchair use. It involves a detailed evaluation of medical conditions, physical capabilities, mental state, and emotional readiness for travel. This comprehensive approach ensures that every factor affecting the patient’s mobility is considered.
A thorough assessment should examine key functional abilities. While this evaluation can be carried out by professionals like physiotherapists, nurses, or caregivers, relying solely on patient or family input may not be enough. Objective tests often provide more accurate insights.
One highly effective tool is the Banner Mobility Assessment Tool (BMAT). This bedside evaluation identifies functional mobility levels and helps determine the type of safe patient handling equipment needed. For instance, BMAT can guide decisions about safe transfers by assessing a patient’s mobility level.
It’s also critical to identify any specialized equipment required for the trip – such as wheelchairs, oxygen tanks, or feeding tubes – and ensure the transport vehicle can accommodate these needs. For longer journeys, consider whether the patient will need extra breaks or more comfortable seating arrangements. Additionally, transport personnel should have access to a doctor’s note outlining the patient’s condition, mobility limitations, allergies, and any other relevant medical details.
This detailed assessment lays the groundwork for efficient scheduling and route planning.
Scheduling and Route Planning
Austin’s traffic and spread-out healthcare facilities make precise scheduling and route planning a must. Leveraging real-time tracking and AI-driven scheduling tools can help minimize delays, reduce missed appointments, and improve overall efficiency [1].
Research backs this up – a 2019 study by Adams Clinical revealed that better transportation access reduced participant dropout rates in clinical trials by up to 20% over two years [1]. Advanced scheduling platforms allow providers to book rides immediately or well in advance, even up to 30 days. These systems are particularly helpful for recurring appointments, such as dialysis or physical therapy sessions. Machine learning can also predict driver availability, making scheduling more reliable [1].
For example, Zyvra Mobility uses AI to navigate Austin’s traffic patterns, ensuring patients arrive on time for their appointments. Dispatchers play a key role here – they need to assign vehicles accurately, communicate effectively with patients who have disabilities, and handle special requests with care.
Once the route is finalized, the next step is confirming that all necessary equipment is ready to go.
Equipment Verification and Documentation
Before hitting the road, it’s crucial to double-check that all required equipment is functioning properly and documented in an up-to-date inventory log. For wheelchairs, ensure every component is working and that the chair fits securely in the vehicle with proper tie-downs or safety straps.
Medical equipment like oxygen tanks, feeding tubes, and monitors must be fully operational, charged, and accompanied by extra supplies. It’s also wise to have a backup plan for wheelchair malfunctions, including spare parts or tools.
Keep a detailed inventory log that includes serial numbers, asset tags, and test results for all equipment. For emergency devices like Automated External Defibrillators (AEDs), perform monthly checks to confirm they’re in "ready status." This includes looking for damage, verifying pads are present and not expired, and ensuring batteries are functional. Don’t forget to pack all necessary medications, along with a list of prescriptions and emergency contact information for caregivers, family members, and healthcare providers.
Comfort is just as important as functionality. Make sure the patient has weather-appropriate clothing in layers, handle any personal hygiene needs before departure, and pack items like cushions, blankets, or pillows to prevent discomfort or pressure sores during the trip. Thoughtful preparation ensures both safety and peace of mind for everyone involved.
sbb-itb-8e5d2ef
During-Trip Safety and Comfort Best Practices
Once the trip is underway, ensuring patient safety and maintaining their dignity takes center stage. Building on the groundwork laid during pre-trip preparations, these practices focus on delivering a safe and comfortable journey. Everything matters – from the vehicle’s condition to the way drivers interact with passengers. Each detail plays a role in shaping the overall care experience during transit.
Vehicle and Equipment Maintenance
All accessible features – like lifts, ramps, securement devices, public address systems, and stop announcement systems – must meet ADA standards. Any malfunctions should be repaired immediately, with temporary solutions provided until full repairs are completed. Routine inspections are essential to catch potential issues before they compromise safety. In Austin’s scorching summers, where temperatures often exceed 100°F, climate controls, lifts, ramps, and securement systems should be tested daily. Vehicles with mechanical issues should be pulled from service until fixed.
Safe Boarding and Securement Procedures
Safe Patient Handling and Mobility (SPHM) programs rely on assistive devices to minimize injuries. Before every transfer, clearly explain the process to patients and seek their cooperation. For wheelchairs, secure tie-downs at all four points. For stretchers, ensure all latches are engaged and add sufficient padding for comfort. These steps not only enhance safety but also demonstrate respect for the patient’s dignity throughout the journey.
Driver Training and Patient Communication
Once pre-trip checks and boarding procedures are complete, the driver’s role becomes critical. Skilled operation of the vehicle and effective communication with passengers are key to ensuring in-transit care. Drivers should be trained in disability-sensitive communication, using person-first language and adapting their approach based on individual needs. For example, they should face hearing-impaired passengers while speaking and verbally announce stops for visually impaired riders.
"Our bus operators are trained to meet the needs of riders with disabilities. If requested, they can assist riders with getting on and off a vehicle and securing wheelchairs. Bus operators are also trained in sensitivity and awareness to meet the needs of riders with disabilities."
At Zyvra Mobility, the focus is on professional and compassionate driver training. Team members are equipped to communicate effectively with passengers who have intellectual disabilities, autism spectrum disorder, or other conditions that may affect how they process information. Considering that 80% of wheelchair users find public transportation challenging to access and use, having empathetic, well-trained drivers makes a significant difference in creating a positive travel experience.
Post-Trip Procedures and Follow-Up
Wrapping up a trip doesn’t mean the job is done. What happens after the ride plays a huge role in ensuring safety and maintaining service quality. The way passengers are handed off and how follow-ups are handled can make or break the overall experience. Clear procedures and thorough follow-ups help create accountability and pave the way for ongoing improvements.
Safe Handover at Destination
The level of service provided determines the type of assistance passengers receive: curb-to-curb (drop-off at the street curb), door-to-door (escorted to the first entrance), or hand-to-hand (direct transfer to a responsible party, ensuring the passenger is never left unattended). For hand-to-hand service, if no attendant is present within five minutes, the driver must keep the passenger onboard and notify dispatch.
Drivers have specific limitations they must follow. For example, they cannot leave the vehicle unattended for long periods, enter beyond the first door of residential buildings, or assist wheelchairs over more than a single step. After the handover, drivers document the trip using the Texas Medicaid Individual Transportation Participant (ITP) Service Record (Form H3017). This form, signed by the receiving healthcare provider or facility staff, confirms that the service was delivered as planned.
Once the handover is complete, the focus shifts to addressing any incidents that occurred and using those lessons to improve future operations.
Incident Reporting and Service Improvement
Every incident – whether it’s a safety concern, equipment issue, or near miss – must be documented within 24 to 48 hours. According to the NHS, serious adverse events occur in up to 10% of hospital admissions, amounting to approximately 850,000 incidents annually. Accurate reporting helps uncover patterns and pinpoint root causes, ultimately reducing the likelihood of repeat issues.
Incident reports should stick to the facts, including details like the date, time, location, what happened, who was involved, any harm caused, and immediate actions taken. Digital tools, such as Zyvra Mobility’s tracking systems, simplify this process by consolidating operational data. These systems make it easier to identify trends and take corrective action. As Prof. Liam Donaldson, WHO Envoy for Patient Safety, aptly put it:
"To err is human, to cover up is unforgivable, and to fail to learn is inexcusable".
Finally, timely follow-ups – through calls or texts within 24 to 48 hours – help close the loop, ensuring passenger satisfaction and providing insights for service improvement.
Conclusion
Transporting patients with mobility challenges in Austin is about more than just getting from point A to point B – it’s about ensuring safety, dignity, and access to crucial healthcare services. By following established best practices, medical appointments become more reliable, and unnecessary complications are significantly reduced. As Texas Senior Care Transport explains:
"Ambulatory transportation is a critical component of the healthcare system, offering a lifeline to many patients who might otherwise struggle to receive the care they need".
Professional Non-Emergency Medical Transportation (NEMT) services play a key role in this process. With trained drivers, ADA-compliant vehicles, and strict adherence to regulations, these providers ensure that patients are transported securely and with the care they deserve. Regular compliance reviews further strengthen the reliability of these services.
In Austin, Zyvra Mobility stands out as a prime example of these principles in action. Their professionally trained drivers, ADA-compliant vehicles, HIPAA-compliant practices, and advanced scheduling tools address many challenges Austin patients face, such as navigating heavy traffic and meeting documentation requirements. The impact of such services is clear: over a two-year period, the US Veterans Health Administration saw 83% fewer missed appointments when professional NEMT services were utilized [1]. Combining regulatory compliance with innovative technology, services like these ensure patients receive the care they need without unnecessary barriers.
Reliable patient transportation doesn’t just improve attendance at appointments – it contributes to better health outcomes, lowers healthcare costs, and enhances overall quality of life. In Austin, it’s a vital part of healthcare delivery, deserving the same level of focus and professionalism as any clinical service.
FAQs
What regulations must NEMT providers in Austin follow?
Non-emergency medical transportation (NEMT) providers in Austin are required to follow a variety of federal, state, and local regulations aimed at ensuring both safety and accessibility. This includes securing the appropriate licenses, adhering to rigorous vehicle safety standards, and meeting driver qualification criteria. Providers must also comply with the operational guidelines established by the Austin Transportation Department and Texas Health and Human Services.
In addition, NEMT vehicles must be equipped to accommodate passengers with mobility challenges. Providers are responsible for keeping detailed records to demonstrate compliance with these regulations. These efforts collectively aim to create a safe and dependable service for passengers.
How can AI tools make scheduling patient transportation in Austin more efficient?
AI-powered tools have the potential to transform patient transportation by simplifying intricate tasks like planning rides and optimizing routes. They can evaluate traffic conditions, forecast delays, and adjust schedules in real time to help ensure patients arrive on time while avoiding unnecessary disruptions.
On top of that, these tools minimize human errors and boost efficiency by leveraging predictive analytics. They can anticipate transportation needs, allocate resources smartly, and improve overall operations. The result? A more seamless and dependable experience for both patients and caregivers.
What transportation challenges do patients with mobility issues face in accessing Austin’s healthcare facilities?
Patients dealing with mobility challenges often encounter major obstacles when trying to access healthcare facilities in Austin. Public transportation is particularly limited in underserved areas, such as eastern and western Austin, where many low-income and uninsured residents reside. For these communities, reaching a hospital or clinic within a reasonable timeframe can feel nearly impossible.
On top of that, problems like inaccessible bus stops, unclear signage, unsafe locations, and insufficient wheelchair-friendly infrastructure make public transit even harder to navigate for those with mobility needs. These barriers can result in delayed medical care, decreased opportunities for social interaction, and poorer health outcomes for some of the city’s most vulnerable residents.